Understanding cycle characteristics
OvuSense is unique. The OvuCore sensor uses Core Body Temperature to predict ovulation using current cycle data, confirm ovulation, and produce detailed cycle patterns which show what is happening to the level of progesterone throughout each cycle. The OvuFirst sensor uses skin temperature to confirm the date of ovulation. The standard version of the OvuSense App can be used with either sensor to track ovulation, and observe cycle patterns by eye.
OvuSense® Pro provides in-depth cycle pattern analysis, automatically flagging each cycle pattern type identified below, aiding diagnosis and treatment of ovulatory issues.
OvuSense Users can purchase OvuSense® Pro as a subscription upgrade, and then share their data with their doctor if they want to. The user and their doctor access the unique insights of OvuSense® Pro through a dedicated encrypted online portal.
Click on each of the cycle pattern images below to find out more - for each image we answer the questions:
- What is it?
- How common is it?
- Why does it happen?
- How can I see it?.
- What does it mean?
- What can be done about it?
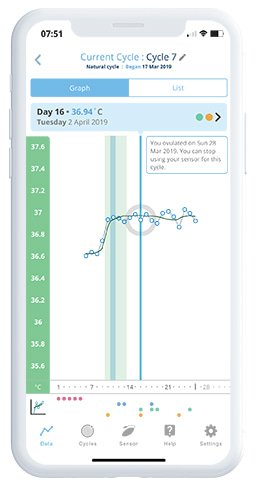
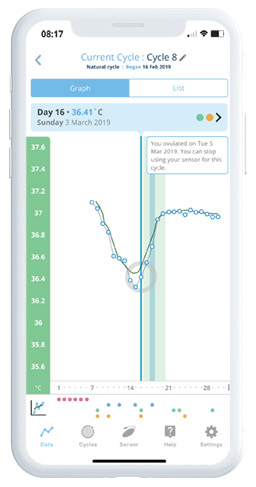
Early Ovulation
What is it?Ovulation that occurs less than 40% of the way through a cycle. That's equivalent to ovulation on day 11 or earlier in a 28 day cycle. It generally results in a shortened 'follicular phase' - which is the time from the start of the period until the day of ovulation in a cycle.
How common is it?
Wilcox et al. (2000) estimated that 2% of women were in their fertile window by the fourth day of their cycle and 17% by the seventh day (based on 213 women).
Why does it happen?
'Early ovulation' is more common the older a woman gets, and simple things like stress, coming off the contraceptive pill, or a recent pregnancy can also cause early ovulation. However, for some women it's just 'their normal'. Klein et al. (2002) - study size 31 explains that the pattern of shortened follicular phase is more frequently identified in older women due to earlier dominant follicle selection as a result of hormonal patterns.
How can I see it?
'Early ovulation' is easy to see using OvuSense due to its real time ovulation prediction and 99% accurate ovulation confirmation. When 'early ovulation' is found, OvuSense® Pro automatically flags this for the user and their clinician.
What does it mean?
It's not necessarily a problem or associated with infertility, but if ovulation commonly occurs very early in the cycle it is something that needs to be discussed with a fertility specialist. Early ovulation has also been found to correlate with a history of recurrent miscarriage - Jukic et al. (2007) - study size 201
What can be done about it?
Having sex in the first days of the cycle after the period has ended is not common for all couples, but will help improve chances of getting pregnant if ‘early ovulation’ is occurring. If that doesn't help with conception, a fertility specialist may recommend drug treatment to 'even' out the cycle and cause ovulation to occur later, and they can also help advise on reducing the risk of miscarriage.
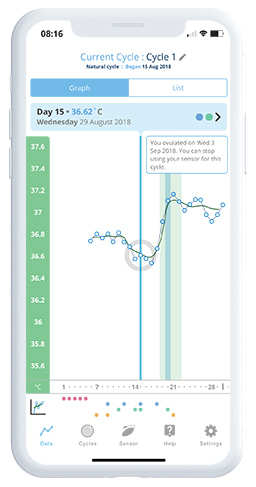
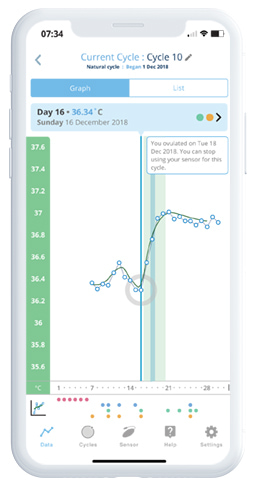
Late Ovulation
What is it?Ovulation that occurs more than 67% of the way through a cycle. That's equivalent to ovulation on day 19 or later in a 28 day cycle. It can sometimes result in a shortened 'luteal phase' - which is the time from the day of ovulation until the first day of the next period.
How common is it?
Hurst B, Citron C (2020) - 15,332 ovulatory cycles from 6,365 OvuSense users showed that 27% of OvuSense users have 'late ovulation'. Hurst B, Davies K (2022) - 158 cycles showed that 34% of cycles in a side-by-side study of OvuCore vaginal and OvuFirst skin-worn sensors in a population with known ovulation issues had late ovulation. These figures appear to be consistent with the findings of Wilcox et al. (2000).
Why does it happen?
'Late ovulation' is often associated with Polycystic Ovarian Syndrome (PCOS) and an under-active or over-active thyroid. Like 'early ovulation' it is also sometimes related to simple things like stress, age or other medications you may be taking. However, just like 'early ovulation' it may just be 'normal' for some women
How can I see it?
'Late ovulation' is easy to see using OvuSense due to its real time ovulation prediction and 99% accurate ovulation confirmation. When 'late ovulation' is found, OvuSense® Pro automatically flags this for the user and their clinician.
What does it mean?
Late ovulation' is not necessarily a problem, or associated with infertility. However, if it results in a consistent short luteal phase (see the separate cycle pattern discussion) from cycle to cycle, then a fertility specialist should be consulted.
What can be done about it?
Having sex later in the cycle will help improve chances of getting pregnant if 'late ovulation' is occurring. If that doesn't help with conception, a fertility specialist may recommend a diet change and/ or drug treatment to 'even' out the cycle and cause ovulation to occur later. The treatment may be different if you just have 'late ovulation' that doesn't cause a short luteal phase.
Anovulation
What is it?When no ovulation occurs in a cycle it is known as 'anovulation' - literally 'without ovulation'.
How common is it?
Although 'anovulation' often occurs with irregular periods (oligomenorrhoea) or an absence of periods (amenorrhoea), it is not uncommon for women with regular periods to have an occasional undetected cycle where they don't ovulate. Hurst B, Davies K (2022) - 158 cycles, showed that 23% of cycles in a side-by-side study of OvuCore vaginal and OvuFirst skin-worn sensors in a population with known ovulation issues were anovulatory.
Why does it happen?
There are many possible causes of 'anovulation' but the most common causes are being underweight (due to excessive exercise and/ or diet), overweight, ovulatory issues such as Polycystic Ovarian Syndrome (PCOS), or physical issues with the ovaries. However, it's important to understand there is a spectrum from having no ovulation at all through to just occasional 'anovulation' and so the treatments vary too.
How can I see it?
OvuSense will display an 'ovulation not detected' message when no ovulation has been seen in a cycle, either through the prediction or detection algorithms. If OvuSense predicts ovulation during a cycle but then doesn't confirm it with the detection algorithm, it will display the message 'ovulation not confirmed'. The difference is important as 'anovulation' patterns can vary greatly. Generally there is some rise and fall in temperature in every cycle, rather than a completely 'flat' line. When 'anovulation' is found, OvuSense® Pro automatically flags this for the user and their clinician but will add additional flags such as 'slow rise' which helps diagnose the cause of the lack of ovulation.
What does it mean?
Frequent lack of ability to ovulate is obviously likely to cause infertility because of the inability to conceive during those cycles. Generally the advice of a fertility specialist should be sought if two in three cycles results in no detected or confirmed ovulation by OvuSense.
What can be done about it?
'Anovulation' of all types can be treated on the advice of a doctor. Hamilton-Fairley D, Taylor A (2003) state, 'Many of the treatments are simple and effective, so couples may need only limited contact with doctors'.
Short Luteal Phase
What is it?The luteal phase is the time from the day of ovulation to the first day of the next period. If this time between ovulation and the next period is 10 days or less, this is normally viewed as a 'short luteal phase'.
How common is it?
Crawford NM, Pritchard DA (2017) - study size 1,635 cycles from 284 women showed that a 'short luteal phase' occurred in 18% of cycles in a group of women with no diagnosis of infertility. OvuSense internal data indicates 25% of users have a luteal phase of 10 days or less.
Why does it happen?
The 'short luteal phase' is commonly seen at times of stress or due to other conditions such as thyroid disorders, Polycystic Ovarian Syndrome (PCOS), and when you start to enter peri-menopause. It can also occur more often in smokers according to Crawford NM, Pritchard DA (2017).
How can I see it?
Only OvuSense can accurately show your luteal phase length because of its 99% accurate ovulation confirmation For best results use OvuSense® Pro, which will automatically flag a 'short luteal phase' for the user and their clinician when found.
What does it mean?
The 'short luteal phase' can lead to the inability to conceive, but more commonly in fact results in a failure of implantation once the egg has become fertilized. For this reason it also carries a high risk of miscarriage and if it occurs in two or more cycles out over a period of six months that would be an indication to consult with a fertility specialist.
What can be done about it?
The good news is that it can be treated relatively easily by your fertility specialist, and OvuSense® Pro can help the user and their clinician to monitor results.
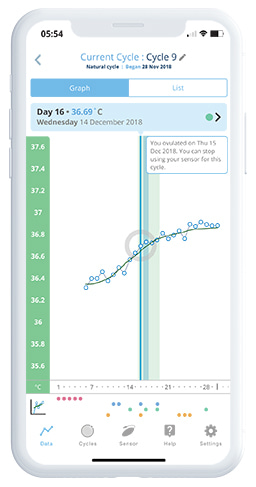
Slow Rise
What is it?Established in the clinical literature by Gautray et al. (1981), a 'slow rise' is characterised by a slow and steady increase in temperature over a number of days, rather than the steep rise over two to three days that is expected with 'normal' ovulation. Some slow rises are the result of ovulation but it is unknown how many, and it is generally taken as an indication that normal ovulation is not occurring.
How common is it?
A 'slow rise' occurs in an estimated 5% of OvuSense users.
Why does it happen?
A 'slow rise' is generally related to Polycystic Ovarian Syndrome (PCOS) and/ or an indication of Polycystic Ovaries (PCO). However, it can also be a sign of Diminished Ovarian Reserve (DOR) which happens as the peri-menopause starts. It is a sign that progesterone is being released more slowly during the process of ovulation, either because the ovaries are 'struggling' to release an egg or because of a hormonal imbalance.
How can I see it?
OvuSense® Pro flags slow rises for the user and their clinician according to a set of mathematical criteria, and although the rise can be seen by eye that doesn't allow reliable classification for the purposes of diagnosing an issue.
What does it mean?
A recurrent slow rise over three or more cycles without a previous diagnosis of either PCOS or DOR would indicate the need for a formal diagnosis.
What can be done about it?
As explained above a recurrent 'slow rise' can be the sign of an underlying ovulatory issue. Those issues can be treated by a number of methods that restore a more rapid release of progesterone during ovulation (which will result in a 'normal' rapid temperature rise).
Crash to Baseline™
What is it?'Crash to Baseline' is a novel cycle pattern characterised in Hurst B, Pirrie A (2019), where temperature (and therefore progesterone) was observed to start at a high level in the cycle, then fall before rising again during ovulation.
How common is it?
Hurst B, Pirrie A (2019) showed that it occurs in 14.2% of total cycles from 20.3% of OvuSense users, so it is a very common cycle characteristic that doesn't follow a typical pattern.
Why does it happen?
As a 'Crash to Baseline' suggests high progesterone early in the cycle. Hurst B, Karoshi M (2020) indicates that it is a particularly strong indicator of PCOS in women with regular cycles (a group that is much less likely to be otherwise diagnosed with PCOS). Hurst B, Karoshi M (2020) also shows a strong association between this pattern women that developed Gestational Diabetes and Gestational Hypertension and this cycle pattern.
How can I see it?
Crash to Baseline indication is only available with OvuSense® Pro, which will flag each cycle with this pattern to the user and their clinician.
What does it mean?
If this pattern occurs in two out of three cycles then it is an indication for a formal diagnosis of PCOS if one hasn't already been made. If this cycle pattern is seen before a pregnancy occurs it can also flag to a clinician that the user should be observed for signs of Gestational Diabetes and Gestational Hypertension during pregnancy, which can be treated more effectively if known in advance.
What can be done about it?
The good news is treatment for PCOS should result in the pattern occurring less often or helping it to disappear. OvuSense® Pro can be used to monitor the effectiveness of the treatment. The advance warning about Gestational Diabetes and Gestational Hypertension risk can also help indicate whether treatment may be needed in pregnancy.
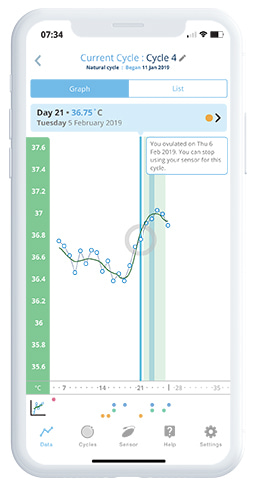
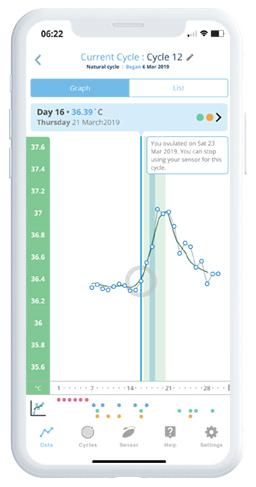
False Start™
What is it?'False Start' is a novel cycle pattern characterised in Hurst B, Pirrie A (2019), where temperature rises around the midpoint in the cycle but isn't as a result of ovulation, and then ovulation occurs at a later point in the cycle.
How common is it?
Hurst B, Pirrie A (2019) showed that it occurs in 9.4% of total cycles from 14.1% of OvuSense users, so it is a relatively common cycle characteristic that doesn't follow a typical pattern.
Why does it happen?
The 'false start' indicates the ovaries are 'trying to release an egg' but failing initially. The temperature curve indicates an initial rise of progesterone, which falls and then rises strongly again at the point of ovulation. Hurst B, Karoshi M (2020) shows this pattern is strongly associated with PCOS, and relatively strongly for those that had a previous miscarriage.
How can I see it?
False Start indication is only available with OvuSense® Pro, which will flag each cycle with this pattern to the user and their clinician.
What does it mean?
If this pattern occurs in two out of three cycles then it is an indication for a formal diagnosis of PCOS if one hasn't already been made. If this cycle pattern is seen before a pregnancy occurs it can also flag to a clinician that the user should be considered for treatment to reduce the risk of miscarriage.
What can be done about it?
The good news is treatment for PCOS should result in the pattern occurring less often or helping it to disappear. OvuSense® Pro can be used to monitor the effectiveness of the treatment. A fertility specialist can also advise on appropriate treatment to reduce the risk of miscarriage.
Crash after Ovulation™
What is it?'Crash after Ovulation' is a novel cycle pattern characterised in Hurst B, Pirrie A (2019), where temperature (and therefore progesterone) was observed to fall rapidly after ovulation before the onset of the next period.
How common is it?
Hurst B, Pirrie A (2019) showed that it occurs in 12.0% of total cycles from 16.0% of OvuSense users, so it is a common cycle characteristic that doesn't follow a typical pattern.
Why does it happen?
As it suggests high progesterone falling after ovulation, it is thought to be associated with Luteal Phase Insufficiency (LPI) where that is not caused by a 'short luteal phase'. LPI is known to be related to a risk of miscarriage Hurst B, Karoshi M (2020) shows a strong association with those that had a previous miscarriage, and internal data from the ongoing OvuSense clinical study confirms a strong association with endometriosis.
How can I see it?
Crash after Ovulation indication is only available with OvuSense® Pro, which will flag each cycle with this pattern to the user and their clinician.
What does it mean?
If this pattern occurs in one or more cycles then it is an indication for consultation regarding the risk of miscarriage, and a formal diagnosis of PCOS if one hasn't already been made.
What can be done about it?
The good news is that treatment for the risk of miscarriage should show an improvement in this cycle pattern, and OvuSense® Pro can therefore be used to assess whether the risk has been reduced by treatment.